Resource center
Explore expert-backed tips, tools, and programs designed to help you stay independent, active, and confident.
Filter by
Physical activity for seniors: Benefits, guidelines, and how to start safely
Discover the benefits of physical activity for seniors, including CDC guidelines, safety tips, and how to start exercising at any age.
Better sleep for seniors: 8 simple habits to improve sleep quality
Discover 8 simple habits to improve sleep for seniors. Learn why sleep is important for older adults, how aging affects rest, and practical tips to boost sleep quality, brain health, and overall well-being.
Nutrition for seniors: Your guide to healthy eating as you age
Why is nutrition important for seniors? As we get older, our bodies naturally go through changes that can affect everything from strength and mobility to memory, sleep, and digestion. Changes in our bodies can affect how we use and absorb nutrients,
Brain health and aging: Your questions answered with Dr. Jessica Rexach
Join Dr. Jessica Rexach as she answers key questions on Alzheimer’s, brain health, and how exercise, sleep, and lifestyle support healthy aging.
Weight management for seniors: What you need to know
Maintaining a healthy weight is so important for our health as we age. The bad news is, there’s no “secret” to weight management for seniors. But there’s good news too: Consistent, healthy habits can help, and it’s never too late to start. Bold spoke
3 chair yoga classes you can do from anywhere
Relax and flow with chair yoga classes available through Bold’s online exercise program. Increase flexibility, improve strength, and build mind-body connection in these yoga classes which utilize a chair for support. Here’s a sneak preview of 3 fan-f
Healthy eating tips with Bold trainer and certified nutritionist Meli Kirkwood
Healthy eating is an essential part of maintaining a healthy lifestyle at any age, but many people don’t know where to start. As Bold’s head trainer, I often hear from members who want to know what they should and shouldn’t be eating. While everyone’
Your top 9 questions about Alzheimer’s disease, answered
Get expert answers to 9 common Alzheimer's questions, from symptoms and diagnosis to prevention tips and caregiver resources.
Recovering strong: Navigating illness and injury in your fitness journey
Learn tips to navigate exercise after illness or injury. Discover recovery tips, gentle movement options, and strategies to restart your routine with confidence.
How to keep your summer workout routine: Simple tips and exercises for summer
Discover how to keep your summer workout routine with flexible tips, summer habits, and exercises for summer. Stay consistent, energized, and confident all season long.
How to restart your routine: Your guide to getting back to fitness
Learn how to restart your routine and start working out again with small, sustainable steps. Discover practical tips for getting back to fitness, building consistency, and creating lasting healthy habits.
How to stay active during travel: 4 of the best travel exercises for seniors
Stay active while traveling with simple exercises, stretches, and mobility routines to boost energy, reduce stiffness, and maintain fitness on the go.
Depression and aging: Signs, causes, and treatment
Some people think depression is a normal part of getting older, but this isn’t true. Normal means something is expected, and depression is not an expected part of aging. Aging and depression are often related due to changes in health, cognitive abili
Anxiety in older adults: Symptoms, causes, and treatment options
Anxiety is a common but often overlooked mental health issue in older adults. Many older adults feel anxious because of big life changes or health problems, but anxiety is not just something normal that happens with age. Anxiety disorders are the mos
6 questions about bone health for seniors, answered
Bone health is a concern for many seniors that’s often overlooked. Osteoporosis, a disease that makes bones weak, affects over 10 million Americans. But it’s a “silent disease” that doesn’t show clear symptoms. This means that many seniors don’t real
How seniors can cut back on alcohol
Learn why seniors should reduce alcohol consumption and discover the health benefits. Get practical tips to cut back on drinking and find support resources today.
How to quit smoking: Steps to understand, manage, and succeed
If you’re reading this, you might be thinking about quitting smoking—or maybe you’re supporting someone who is. Smoking remains one of the leading causes of preventable disease and death. Quitting smoking is one of the most important steps you can ta
How to cope with loneliness: Small steps to feel less alone as you age
Feeling lonely is more common than you might think, especially as we get older. You may feel isolated even if you’re not completely alone. Maybe you’ve lost friends or family, moved to a new place, or just don’t have as many chances to connect with o
Dementia and memory loss: Causes, risks, and prevention
Learn the difference between normal aging and dementia. Discover causes, risk factors, prevention strategies, and how exercise protects brain health.
Sex & dating with incontinence: 10 things I wish I knew beforehand
This blog was originally authored by Because, which offers a wide range of bladder protection products that you can easily purchase online and have delivered right to your door in discreet packaging. Get 20% off your first order using the code ‘BOLD2
Pelvic floor exercises for seniors: Building a stronger routine
Did you know that pelvic floor exercises can help you stay healthy as you age? Your pelvic floor muscles help you control when you go to the bathroom, they support your pelvic organs and they play a role in sexual health. Keeping these muscles strong
How to talk to your doctor about balance and fall prevention
As we get older, it's common to start to experience balance changes. These changes can be due to a number of factors, including age-related muscle loss. Changes in our balance can make us more likely to fall. Up to 1 in 4 older adults experience a fa
Talking to your doctor about physical activity: Why it matters & tips to ease conversation
Whether you’re a Bold enthusiast or are just starting a new routine, you’ve taken steps to bring physical activity into your life, and that’s something to be proud of! Being physically active has a big impact on your overall health, from managing chr
How to talk to your doctor about bladder leaks
Struggling with bladder leaks? This guide helps you prepare for doctor visits, find the right specialist, and explore treatment options for urinary incontinence.
Bold fitness equipment guide: What you need for online classes
Bold classes can be done anytime, anywhere — with or without equipment. If you’d like to add equipment into your routine, you’ll see some Bold trainers demonstrate movements with items like bands or hand weights. You can also use substitutes you hav
Your top sleep questions for seniors, answered
Learn how sleep needs change with age from sleep expert Dr. Kimberley Truong. Discover why quality sleep matters for seniors' health, signs of sleep problems, and expert tips for better rest.
Lower back pain: 3 common causes and how to stay active
Lower back pain is one of the most common types of discomfort we experience as we age. Understanding the causes of lower back pain can empower us to manage it effectively and continue living an active, fulfilling life. Here’s a breakdown of the top 3
New year fitness & wellness goals: Where to start
The new year is a great time to set health goals. Here are some ideas for doing just that: 1. Take fitness to the next level Now is the time to take things up a notch—meaning, try things like increasing the number of days that you’re working out, tr
How to adjust your workout routine for hot summer weather
With record temperatures every summer, it’s important to adapt your fitness routine to stay cool and Be Bold. Here are 4 science-backed tips to beat the heat during exercise: 1. Work out in controlled environments (indoors, shaded areas, early mornin
Best time of day to exercise: Morning vs. evening workouts
If you jump out of bed early in the morning, an AM class might be your best bet. On the other hand, if you’re more of a slow riser with a busy workday, PM classes might be your friend. The good news is that regardless of the time of day you choose, B
How to set exercise goals for seniors that actually work
Learn how to set realistic, specific, and meaningful exercise goals for seniors. Discover short-term and long-term fitness goal examples to stay active and motivated at any age.
How to set a goal and create an action plan
Turn fitness goals into reality with a simple 5-step action plan. Learn to assess your baseline, try a program, track progress, and stay motivated.
The best stretches for seniors, explained
Discover the best stretches for seniors including hip stretches for flexibility, balance, and mobility. Learn when to stretch and get expert tips for safe, effective routines.
Bold Guide: Exercise for diabetes management
Discover safe, effective exercise ti[s for diabetes management in older adults. Get blood sugar control tips, workout guidelines, heat safety advice, and more.
Get comfortable: What to do at home to reduce strain as you age
While exercise is essential to better health, there are also several things you can do at home to your space to feel healthier. We sat down with home ergonomics expert Udell Craven on how to set up your living space to reduce strain on the body and
What older adults should add to their exercise program
Most people associate aging with being weak, frail, and declining health. But aging is a natural process — and attitude makes all the difference! One of the changes people typically notice as they age is the loss of muscle mass and weakness. They may
5 reasons why you’re not exercising (and how to deal with them)
Avoiding exercise due to pain, lack of time, or low energy? Discover why you're not exercising and find simple strategies to overcome every barrier.
4 ways to overcome fatigue
Fatigue is one of the most common side effects of illnesses, including heart disease, cancer, rheumatoid arthritis, lung disease, kidney disease, and neurological conditions. It’s more than just being tired; it affects the whole body. Astudy found t
How to prepare for your first Bold class
New to working out or setting up a space to move? The first time trying anything new can be intimidating, which is why we want to make getting started with Bold as easy as possible. Bold brings exercise to you by delivering classes to you online! By
Get Bold: Free online fitness with Renew Active from UnitedHealthcare
Bold is available at no cost to members with Renew Active, the fitness program included in eligible UnitedHealthcare Medicare Advantage plans. Whether you’re looking to improve balance, build strength, or simply stay active at home, Bold’s flexible o
How to sign up for live classes
We started our weekly live classes as a way to connect with the community, and give members a chance to meet Bold’s team of instructors and experts. Thanks to everyone who’s joined us these last couple of months, we’ve designed a new, easier process
How to do a squat
Exercise: The squat Improves: Lower body strength The squat is an extremely beneficial exercise that builds lower body strength by targeting the glutes, quadriceps, and hamstrings. Also, regularly practicing the squat can improve core strength and jo
8 pieces of advice from 77 year old powerlifter Abbey Moon
If there’s one word that comes to mind when describing powerlifter Abbey Moon, it’s determined. The Seattle-based weightlifting champion turned 77 and power lifts multiple times a week at her home gym, hosts Zoom classes with friends, and meets with
5 exercises you can do from your chair
It’s time to forget the myth that you can’t exercise without spending a lot of time on your feet. Seated from a sturdy chair, you can still build strength and improve flexibility. Seated workouts can be a simple, safe, and effective option when you’
How-to videos: 5 chair exercises for seniors
Discover 5 senior-friendly chair exercises to build strength, boost flexibility, and support healthy aging.
4 senior-friendly chair exercise classes
Explore four senior-friendly chair exercise classes from Bold designed to improve balance, strength, and heart health.
Chair sit-ups: Key benefits & how to do them
Chair sit-ups are a safe and effective seated exercise to build core strength, improve posture, and support balance.
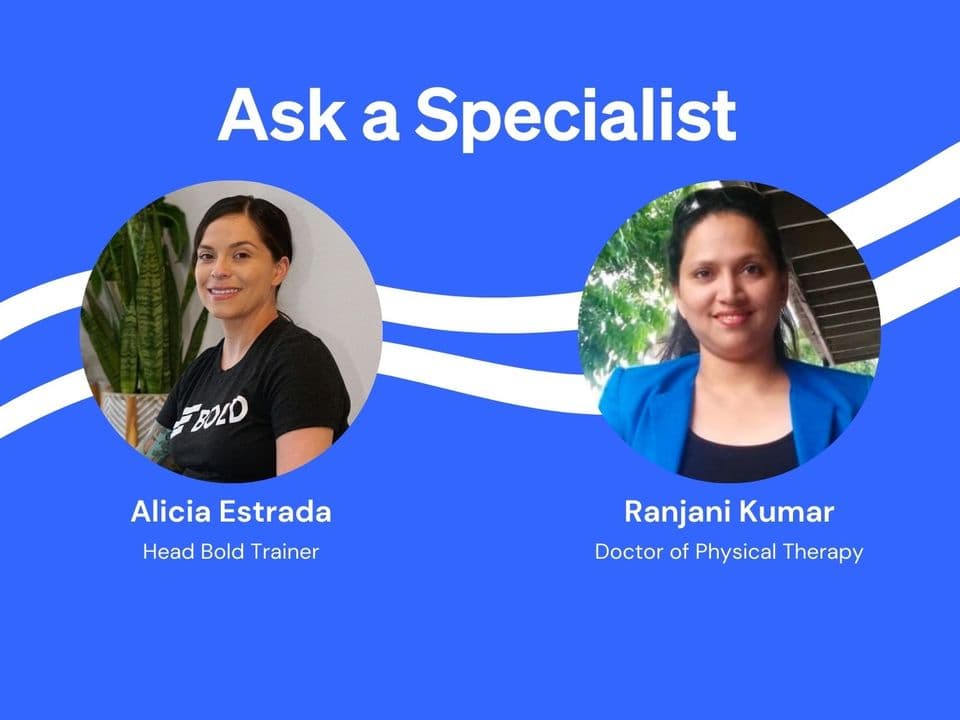
Your questions about healthy aging and balance, answered
Physical therapist Dr. Ranjani Kumar and Bold’s head trainer Alicia Estrada share expert advice on how balance affects healthy aging.
7 benefits of Tai Chi for older adults
Tai Chi is a gentle, powerful way to improve balance, reduce pain, and support healthy aging.
How to practice self-care as you age
Discover five simple, expert-backed ways to reduce stress and feel better every day with Bold.
How to address neck and upper back pain: Top 3 diagnoses and ways to cope
Learn the top causes of neck and upper back pain.
Bladder leaks in seniors: What causes them, and what to do about them
Learn what causes bladder leaks in seniors and how to manage them with lifestyle changes like pelvic floor exercises.
5 of the best sports for seniors
Discover top sports for seniors: golf, tennis, pickleball and more. Stay active, safe, and healthy with age-friendly exercise tips.
Bold Guide: Exercise for pain management
Learn how Bold’s online exercise classes help older adults reduce pain and regain control.
Bold Guide: Exercise and mental health
Mental health matters at every age.
Bold Guide: Exercise for arthritis
Exercise is one of the most effective ways to manage arthritis.
Bold Guide: Exercise for a healthy heart
Learn how Bold’s expert-designed exercise classes can help lower your risk of heart disease and keep you strong for life.
10 reasons why older adults walk with a shuffling gait
Shuffling your feet may seem harmless, but it's a common gait issue that increases fall risk in older adults. Learn the causes and how to correct it with exercise.
Chair workouts for seniors: Your top 5 questions, answered
Discover the benefits of chair workouts for seniors: build muscle, improve balance, and stay safe while seated. Get started with simple exercises at home.
6 foods to eat or avoid to prevent Alzheimer’s disease
Dr. Annie Fenn, physician and founder of Brain Health Kitchen, shares six science-backed food tips to help prevent Alzheimer’s disease and support lifelong brain health.
Brain health for seniors: Tips, exercises, & lifestyle habits for memory and cognition
Discover what seniors need to know about brain health, including cognitive function, memory improvement, and exercises to support brain health as you age. Learn practical tips for maintaining mental sharpness.
Bone health for seniors: Why it matters and how to support it
Learn how bone health changes with age and discover practical tips to prevent osteoporosis. Explore risk factors and learn how lifestyle changes can keep your bones strong.
Fall prevention for seniors: Staying safe, strong, and independent
Fall prevention for seniors starts with balance training. Explore safe exercises, risk factors, and proven tips to stay safe and confident.
How to age in place
Expert aging-in-place tips from a certified specialist. Learn how to plan, modify your home, and stay safe as you age comfortably in the home you love.